Abstrict
Antibiotics cure infectious diseases however; their irrational use may devastate by way of microbial resistance, adverse drug reactions, and or worsening of the diseased conditions. This study is aimed not only to assess the existing loopholes in dispensing antibiotics but also a futuristic appraisal inferencing preparation of graduating pharmacists for good dispensing practices. Therefore, the population included in the study are Pharm D students to appraise their knowledge level and perception regarding antibiotic prescription and dispensing that will serve as key indicators to the community being served. A precondition for the participants was their exposure to infectious diseases and use of antibiotics during pharmacy graduation studies to include a knowledgeable population. A questionnaire was prepared comprising expected breaches during the dispensing and course of treatment with antibiotics, which was sent electronically to the participants. A population of 2500 students was focused on geographic proximity where they may share the common job market in dispensing pharmacies.
Keywords
Graduating Pharmacists, Antibiotic Prescription, Good Dispensing Practices, WHO Indicators
Introduction
Based on its accidental discovery the word antibiotics arose from “anti” meaning against and “bios” life however, presently the terminology is confined to antibacterial drugs. The term “antibiotic” was defined as a substance produced by microorganisms, which inhibits the growth of other microorganisms even in the highest dilutions (Newton et al., 2023). This definition excluded other antibacterial substances like gastric juices or synthetic antimicrobials. Although, in general, all medicines used against microbial infections are termed antibiotics, contrarily, in medical settings, the antibacterial comes from natural sources like microbial fermentation are termed antibiotics e.g. Penicillin, cephalosporin, etc. While those obtained through synthetic reactions are termed non-antibiotic antibacterial antimicrobials like Sulfonamides and antiseptics (Reardon, 2014).
Antibiotics are being widely used in the treatment and prevention of infectious diseases to kill “bactericidal” or inhibit “bacteriostatic” the growth of bacterial cells. Antibiotics have been used since ancient times in the treatment of infectious diseases (Kokare et al., 2007b). Many civilizations reported rubbing moldy breads for topical application but the first document refers to John Parkinson (1567-1650). However, the accidental discovery of Alexander Fleming in 1928 led to the widespread beneficial use of penicillin as an antibacterial drug (Bennett & Chung, 2001). The efficacy against infections and easy access to antibiotics led to irrational use, which appeared in the form of bacterial resistance (Rodríguez-Rojas et al., 2013). Some of the antibiotics are also used in the treatment of protozoal infections.
Although they are not effective in several diseased conditions like viral infections, but still used either to prevent bacterial superinfections or misunderstanding of the symptoms, which always devastate the patient's health (Bozinovski et al., 2020). Sometimes an empiric treatment is initiated by prescribing broad-spectrum antibiotics to treat the signs and symptoms of the disease without knowing the causative organism (Mettler et al., 2007). On the other hand, the prescription of broad-spectrum antibiotics has also led to serious health issues like these are dangerous to the normal flora (Giuliano et al., 1987). Similarly, based on ease of treatment, not only do physicians usually prescribe such drugs but also being misused due to self-medication. The World Health Organization (WHO) has classified bacterial resistance to antibiotics as a serious threat, which appears all the time everywhere affecting anyone regardless of age and gender. As per the global burden of diseases (GBD) 2019, 1.7 M deaths were attributed to resistance against antimicrobial drugs due to failure of treatment until the end.Keeping in view the existing gaps in good dispensing practices of antibiotics and futuristic improvements, undergraduate pharmacy students may be trained and equipped with the essential knowledge to ensure the rational use of antibiotics. Therefore, the current study was designed to assess the perception and knowledge level of graduating pharmacists as a clue to the future of good dispensing practices. The selection of population was based on proximity where the majority of professional pharmacists share the same job market or community and hence serves as a good tool for fair assessment. The findings of this study will serve as a tool for appraising the theoretical knowledge, skills, and aptitude of future pharmacists toward rational use of antibiotic therapy and any necessary modification in curricula to fill the gap.
Research Methodology
Study Area
The study was conducted amongst undergraduate pharmacy students including the Department of Pharmacy, Quaid I Azam
University Islamabad, University of Swabi, Ripha University Islamabad, and Abaseen University Islamabad. The pharmacy departments are located within 200 Km2 graduating 500 pharmacists each year, collectively. Hence, the approximate number of the total population becomes 2500 Pharm D students. The departments are engaged in high-quality research productivity representing a conducive environment for undergraduate students. Besides other professional services like industrial pharmacy, pharmaceutical marketing, teaching & research, many graduates serve the community pharmacy and hospital pharmacy in the twin cities of Islamabad region and other parts of the country sharing the same job market. Some of the pharmacy graduates also prefer to move to neighboring and advanced countries and render their services in pharmacy setups.
Study Design and Time-Period
A cross-sectional study was conducted from October to December 2023 amongst the undergraduate students of the Pharm D program.
Source and Population
The source of the population for this assessment were various pharmacy departments offering Pharm D programs in proximity based on geographical location and students who faced some infectious
diseases during graduation. The study population was currently enrolled Pharm D students who personally experienced a course of antibiotic treatment duly prescribed by the physicians and subsequently obtained from the nearby pharmacies. The study area covered the location of students but not the site of hospitals or clinical setups from where they got prescriptions and prescribed medication. Furthermore, an interview was also conducted to know the problem with reasons for problems associated with the correct posology, indications, usage, and drug identification that may have any potential hindrance in the course of treatment.
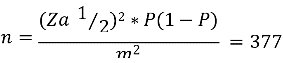
Sampling Procedure and Size Determination
All undergraduate Pharm D students were included in the study with a precondition of exposure to any infectious diseases during graduation studies. The sample size of participants was calculated employing a single-population-proportion equation and a factor of finite-population-correction, given as under.
Where “n” represents the size of the sample from the equation, “Za 1?2” represents a 95% confidence level, “P” is the population of participants, and “m” margin of error (5% = 0.005) ("Finite Population Correction (FPC) Factor,” 2008).
Before deciding the final sample size, the authors reviewed the exposure level based on responses received from various participants to determine the number of encounters during
the course of graduation. As per a random survey before starting the actual study, it was deduced that more than 90% of the undergraduate students were exposed to some kind of infectious disease. Based on environmental conditions of the region and length of study in the graduation program which approximately becomes 2250 students. Therefore the sample size obtained from the equation en-1 (n= 377) was corrected with the finite-population-correction factor as a sampling frame for 2250 was <10000 given as under.
Where “??” represents the adjusted sample size of (n= 377) and “N” refers to the population.
Procedure for Data Collection
Observational technique was employed in the collection of data also followed by an interview of the participating students where appropriate. A checklist-based Google form questionnaire was prepared for the collection of observational data and student interviews respectively. The questionnaire was sent electronically to participants to avoid bias in observational data collection, which may occur during physical interaction and ensuing willful participation. Observational data collection technique was employed to evaluate awareness about the use of antibiotics, preference of use, knowledge about use in viral infections, drug-food interaction, completion of a course of treatment, guidance to patient, and self-medication by keeping antibiotics at home.
Data Curation and Analysis
Statistical evaluation was performed using MS Excel broadsheet by extracting data from Google Forms. After adjusting the outliers, coding, and entering the data in a broadsheet statistical analysis was performed and results were presented using a graphical presentation comprising frequency of occurrence, percentage of the population, mean, and standard error of the mean of the data. Regression was also applied to determine the association between subject knowledge about dosage regimen, sociodemographics, and other factors related to the end user of antibiotics.
Quality Assurance of Data
A pretest survey was conducted on 10% of the sample size by comprising a demographic population to evaluate the completeness of the required questionnaires as a data collection tool and the expected time that would be required for the study. The principal investigator offered detailed training about data collection, handling, and subsequent evaluation based on the objectives of the study and its significance to good dispensing practices. The data collecting team regularly checked and evaluated the completeness of the data.
Operational Definitions
Awareness about the use of antibiotics: To evaluate the rational use of antibiotics in case of bacterial infections or to prevent bacterial superinfections but avoid other infectious conditions like viral infections.
Preference of use: How often the antibiotics are preferred to be used without knowing the exact microorganism, prophylactic treatment, or waiting for the immune response like the use of probiotics in case of gastric infections.
Knowledge about use in viral infections: If the antibiotics are often used during infections like influenza, shingles, measles, etc.
Drug-food interaction: Being a knowledgeable end user whether the graduating pharmacists have basic knowledge of drug-food interaction, which not only alters the efficacy but greatly correlates with the absorption and consequent bioavailability issues.
Completion of a course of treatment: To know if the subjects are aware of the importance of the course of treatment and microbial resistance in case of incomplete treatment.
Guidance to patient: Whether the subjects were guided by the dispensing pharmacist regarding storage conditions, correct dosage, handling, and reporting of side effects, as key indicators to identify gaps in good dispensing practices.
Self-medication by keeping antibiotics at home: Keeping antibiotics at home indicates self-medication of the drugs, which may appear in the form of misuse of antibiotics.
Results
Sociodemographic Characteristics of the Pharmacy Students
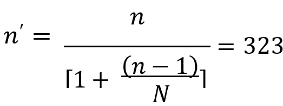
A total of undergraduate students took part in the study resulting in a response rate of 100%. Out of the total number of students, more than half were male students (67.1%) and 32.9% of students were female. Most of the students were 21 – 30 years of age (75.2%) however, 22.8% were below 20 years of age and 2% were aged 31 – 40 years. Most of the students were unemployed (91.9%) and only a few were employed (8.1%).
Figure 1
Question Title: Gender
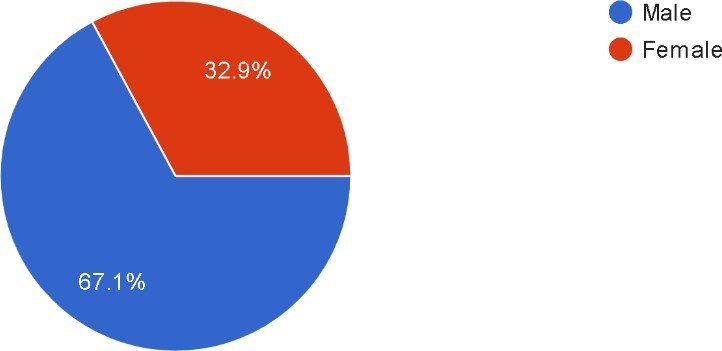
Figure 2
Question Title: Age
Table
1:
Sociodemographic characteristics of undergraduate pharmacy
students.
|
Sociodemographic characters |
Percentage Frequency |
|
Gender female Male |
32.9% 67.1% |
|
Age (years) Below 20 21 – 30 31 – 40 Above 40 |
22.8% 75.2% 2.0% 0% |
|
Occupation Employed Unemployed |
8.1% 91.9% |
All of the students i.e. 100%
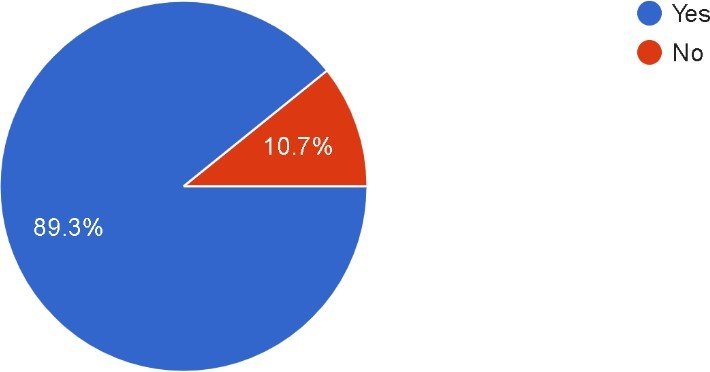
were aware of antibiotic drugs but 96% of students were aware of their rational use. 89.3% of students preferred the use
of antibiotics in case of infection while
10.7% of students did not prefer the use of antibiotics at early stages of
infection. 67.1% of students were
aware of the usefulness of antibiotics in case of bacterial infections while
30.2% of students believed
that antibiotics are not useful
in case of bacterial infections. 75.2% of the students
considered antibiotics useful in
case of viral infections while 24.8% of
students were unaware of their
use in viral infections.
Figure 3
Question title: Do you know what antibiotics are used for?
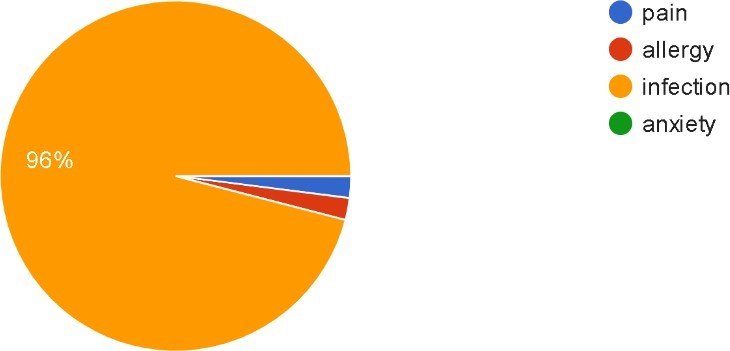
Figure 4
Question title: Do you prefer the use of antibiotics in case of any infection?
Knowledge Provided by the Pharmacist About the Prescribed Antibiotics.
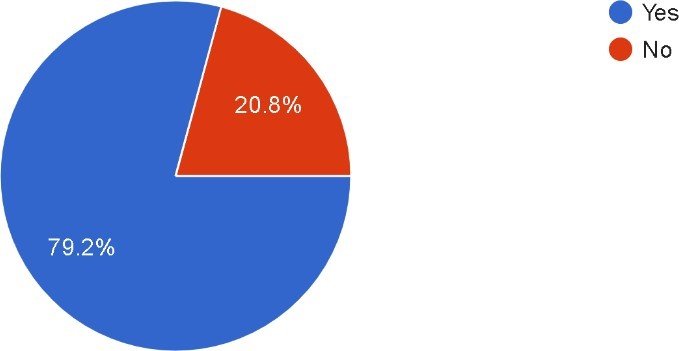
79.2% of students completed the course of antibiotics as prescribed while 20.8% of students did not complete the course as prescribed which shows that most students were aware of the bacterial resistance which may result in an incomplete course of treatment. 77.9% of students were provided with basic knowledge about the prescribed antibiotics. The knowledge provided to patients about a dose of antibiotic was 68.5%, route of administration (47.7%), frequency of medication (39.2%), and side effects (44.6%). 46.3% of students would sometimes forget about the instructions provided by the pharmacist, 15.4% often forgot the instructions 32.9% would never forget about the instructions and few students responded that they always forgot the instructions. 85.9% were aware of the conditions in which the antibiotics are kept at home while some (14.1%) remained unaware.
Figure 6
Question title: Did you complete the course of medication as prescribed?
Discussions
The study evaluated the knowledge and perceptions of graduating pharmacists regarding prescribed antibiotics, focusing on awareness, preferences, and good dispensing practices. The findings offer valuable insights into the current understanding and potential areas for improvement among future pharmacists.
The study shows a high level of awareness about antibiotics among graduating pharmacists, with all participants acknowledging their existence and 96% understanding their rational use. This indicates effective education on the fundamentals of antibiotics. However, the 4% lacking this knowledge highlights the need for continuous educational efforts to ensure comprehensive understanding among all students.
Most students (89.3%) preferred using antibiotics in infection cases, indicating a reliance on these drugs. However, 10.7% did not favor early antibiotic use, reflecting a more cautious approach. This aligns with best practices to avoid unnecessary antibiotic use and mitigate resistance development.
A significant misconception was noted, with 75.2% of students considering antibiotics useful for viral infections like influenza, shingles, and measles. This incorrect belief underscores a critical area for educational improvement. Antibiotics are ineffective against viruses, and their misuse can contribute to antimicrobial resistance and public health issues. Addressing this gap is essential for fostering appropriate antibiotic use.
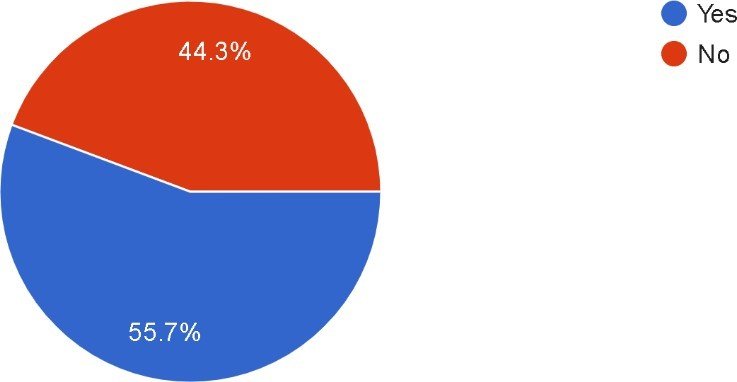
The study found that 55.7% of students were aware of antibiotic-food interactions. Many students correctly identified that tetracyclines should not be taken with milk due to reduced absorption. Additionally, there was a belief that antibiotics should generally be taken before meals to avoid absorption issues, though this varies by antibiotic type. For instance, azithromycin should be taken before meals. While this understanding is encouraging, nearly half of the students were not fully informed, indicating a need for enhanced education on food-drug interactions.
Awareness of the importance of completing antibiotic courses was high, with 79.2% of students adhering to prescribed courses. This suggests a good understanding of the risks of bacterial resistance from incomplete treatment. However, the 20.8% who did not complete their courses highlight the need for reinforcing adherence to treatment regimens.
Effective patient counseling is vital for good dispensing practices. The study revealed that 77.9% of students received basic information about prescribed antibiotics from pharmacists. However, more detailed guidance on dosage, route of administration, frequency, and side effects was less frequently communicated (68.5%, 47.7%, 39.2%, and 44.6% respectively). Additionally, 46.3% of students sometimes forgot pharmacist instructions, and 15.4% often forgot them. This suggests that while initial communication occurs, its effectiveness is limited, indicating a need for strategies to enhance patient recall and understanding.
The tendency towards self-medication, indicated by storing antibiotics at home, poses misuse risks. The study found that 85.9% of students were aware of appropriate storage conditions, while 14.1% were not. Proper storage awareness is critical to prevent misuse and ensure antibiotics remain effective until needed.
Conclusion
The study indicates that while graduating pharmacists have a solid foundational knowledge of antibiotics, significant misconceptions and gaps remain, especially regarding their use in viral infections and principles of antibiotic stewardship. Addressing these gaps through targeted educational initiatives is crucial for preparing future healthcare professionals to combat antimicrobial resistance and ensure safe and effective antibiotic use. Emphasizing patient guidance, treatment course completion, understanding antibiotic-food interactions, and avoiding self-medication can further enhance good dispensing practices. Ensuring pharmacists can provide comprehensive information on storage conditions, correct dosages, and side effect management is vital for optimizing treatment outcomes and patient safety.
In summary, continuous education and strategic improvements in training programs are essential to equip future pharmacists with the necessary knowledge and skills to manage antibiotics effectively, ensuring better healthcare outcomes and minimizing the risks of antibiotic misuse and resistance.
References
-
Newton, D. P., Ho, P., & Huang, K. C. (2023b). Modulation of antibiotic effects on microbial communities by resource competition. Nature Communications, 14(1). https://doi.org/10.1038/s41467-023-37895-x
- Reardon, S. (2014b). Antibiotic resistance sweeping the developing world. Nature, 509(7499), 141–142. https://doi.org/10.1038/509141a
- Kokare, C., Chopade, B., Mahadik, K., Martin, C., Aery, S., Hargun, N., Bhujbal, U., & Kenward, M. (2007c). Pharmaceutical microbiology. Journal of Pharmacy and Pharmacology, 59(Supplement_1), A-19. https://doi.org/10.1211/002235707781850078
- Bennett, J. W., & Chung, K. (2001b). Alexander Fleming and the discovery of penicillin. In Advances in applied microbiology (pp. 163–184). https://doi.org/10.1016/s0065-2164(01)49013-7
- Rodríguez-Rojas, A., Rodríguez-Beltrán, J., Couce, A., & Blázquez, J. (2013b). Antibiotics and antibiotic resistance: A bitter fight against evolution. International Journal of Medical Microbiology, 303(6–7), 293–297. https://doi.org/10.1016/j.ijmm.2013.02.004
- Bozinovski, S., Aloe, C., & Wang, H. (2020b). Viral-Induced Bacterial Superinfections Drive Emergence of an Immunosuppressive Neutrophil Phenotype. https://doi.org/10.1164/ajrccm-conference.2020.201.1_meetingabstracts.a1178
- Mettler, J., Simcock, M., Sendi, P., Widmer, A. F., Bingisser, R., Battegay, M., Fluckiger, U., & Bassetti, S. (2007b). Empirical use of antibiotics and adjustment of empirical antibiotic therapies in a university hospital: a prospective observational study. BMC Infectious Diseases, 7(1). https://doi.org/10.1186/1471-2334-7-21
- Giuliano, M., Barza, M., Jacobus, N. V., & Gorbach, S. L. (1987b). Effect of broad-spectrum parenteral antibiotics on the composition of intestinal microflora of humans. Antimicrobial Agents and Chemotherapy, 31(2), 202–206. https://doi.org/10.1128/aac.31.2.202
-
Finite Population Correction (FPC) factor. (2008b). Encyclopedia of Survey Research Methods. https://doi.org/10.4135/9781412963947.n191
-
Newton, D. P., Ho, P., & Huang, K. C. (2023b). Modulation of antibiotic effects on microbial communities by resource competition. Nature Communications, 14(1). https://doi.org/10.1038/s41467-023-37895-x
- Reardon, S. (2014b). Antibiotic resistance sweeping the developing world. Nature, 509(7499), 141–142. https://doi.org/10.1038/509141a
- Kokare, C., Chopade, B., Mahadik, K., Martin, C., Aery, S., Hargun, N., Bhujbal, U., & Kenward, M. (2007c). Pharmaceutical microbiology. Journal of Pharmacy and Pharmacology, 59(Supplement_1), A-19. https://doi.org/10.1211/002235707781850078
- Bennett, J. W., & Chung, K. (2001b). Alexander Fleming and the discovery of penicillin. In Advances in applied microbiology (pp. 163–184). https://doi.org/10.1016/s0065-2164(01)49013-7
- Rodríguez-Rojas, A., Rodríguez-Beltrán, J., Couce, A., & Blázquez, J. (2013b). Antibiotics and antibiotic resistance: A bitter fight against evolution. International Journal of Medical Microbiology, 303(6–7), 293–297. https://doi.org/10.1016/j.ijmm.2013.02.004
- Bozinovski, S., Aloe, C., & Wang, H. (2020b). Viral-Induced Bacterial Superinfections Drive Emergence of an Immunosuppressive Neutrophil Phenotype. https://doi.org/10.1164/ajrccm-conference.2020.201.1_meetingabstracts.a1178
- Mettler, J., Simcock, M., Sendi, P., Widmer, A. F., Bingisser, R., Battegay, M., Fluckiger, U., & Bassetti, S. (2007b). Empirical use of antibiotics and adjustment of empirical antibiotic therapies in a university hospital: a prospective observational study. BMC Infectious Diseases, 7(1). https://doi.org/10.1186/1471-2334-7-21
- Giuliano, M., Barza, M., Jacobus, N. V., & Gorbach, S. L. (1987b). Effect of broad-spectrum parenteral antibiotics on the composition of intestinal microflora of humans. Antimicrobial Agents and Chemotherapy, 31(2), 202–206. https://doi.org/10.1128/aac.31.2.202
-
Finite Population Correction (FPC) factor. (2008b). Encyclopedia of Survey Research Methods. https://doi.org/10.4135/9781412963947.n191
Cite this article
-
APA : Manal, N., Noor, H., & Arshad, A. (2023). Knowledge and Perception of Graduating Pharmacists about Prescribed Antibiotics as a Futuristic Appraisal of Good Dispensing Practices. Global Pharmaceutical Sciences Review, VIII(IV), 49-56. https://doi.org/10.31703/gpsr.2023(VIII-IV).05
-
CHICAGO : Manal, Nazzaha, Hira Noor, and Anam Arshad. 2023. "Knowledge and Perception of Graduating Pharmacists about Prescribed Antibiotics as a Futuristic Appraisal of Good Dispensing Practices." Global Pharmaceutical Sciences Review, VIII (IV): 49-56 doi: 10.31703/gpsr.2023(VIII-IV).05
-
HARVARD : MANAL, N., NOOR, H. & ARSHAD, A. 2023. Knowledge and Perception of Graduating Pharmacists about Prescribed Antibiotics as a Futuristic Appraisal of Good Dispensing Practices. Global Pharmaceutical Sciences Review, VIII, 49-56.
-
MHRA : Manal, Nazzaha, Hira Noor, and Anam Arshad. 2023. "Knowledge and Perception of Graduating Pharmacists about Prescribed Antibiotics as a Futuristic Appraisal of Good Dispensing Practices." Global Pharmaceutical Sciences Review, VIII: 49-56
-
MLA : Manal, Nazzaha, Hira Noor, and Anam Arshad. "Knowledge and Perception of Graduating Pharmacists about Prescribed Antibiotics as a Futuristic Appraisal of Good Dispensing Practices." Global Pharmaceutical Sciences Review, VIII.IV (2023): 49-56 Print.
-
OXFORD : Manal, Nazzaha, Noor, Hira, and Arshad, Anam (2023), "Knowledge and Perception of Graduating Pharmacists about Prescribed Antibiotics as a Futuristic Appraisal of Good Dispensing Practices", Global Pharmaceutical Sciences Review, VIII (IV), 49-56
-
TURABIAN : Manal, Nazzaha, Hira Noor, and Anam Arshad. "Knowledge and Perception of Graduating Pharmacists about Prescribed Antibiotics as a Futuristic Appraisal of Good Dispensing Practices." Global Pharmaceutical Sciences Review VIII, no. IV (2023): 49-56. https://doi.org/10.31703/gpsr.2023(VIII-IV).05
